55years old patient with seizures.
May 12 , 2021
Student- A. Rishi koundinya
Batch- 2017
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
A 55year old male patient came to opd with c/o altered sensorium and involuntary movements from 11pm and recurrent episodes of seizures since 5yrs.
Patient is apparently asymptomatic before 5years and there is a history of fall on road while running and there is a injury to head , visiting to hospital near nalgonda and after investigation it is diagnosed as a brain stroke , the first episode of seizures had started there and then they have shifted to AMMA Hospitals and treatment is being taken.
Inspite of treatment there are recurrent episodes of seizures like nearly 15 episodes in 5 years.
They are incidious in onset and started with folding of fist and Tremors in the left leg and slowly progress all over the body and they are predominantly on left side of the body.It is associated with frothing, tongue biting, eye rolling, and patient is conscious. Duration of seizures is for 10 to 20min, Relieved on medication, triggered by stress.
In the recent episode continuous tonic clonic movements from 11pm to 2am there is also loss of consciousness and slurred speech and deviation of mouth.
He also had a defect in vision of left eye after the injury.
Post ictal stage is associated with headache, weakness .
He is k/c/o HTN since years and on medication.
Not a k/c/o of DM, ASTHMA, TB.
He had mixed diet with normal Appetite, adequate sleep , regular bowel and bladder movements. Had a habit of alcohol regularly 90ml/ day and stopped after the accident.
EXAMINATION:
Patient was drowsy , and not well oriented to time place.
There are no signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, edema.
VITALS - At time of presentation
Bp-220/120
Pr-110
Cvs- s1 s2+
Respiration-22
breath sounds decreased in bilateral infra axillary areas
Cns patient was drowsy at time of presentation.
VITALS - Today morning
bp - 120/80
Pr - 92
Cvs - s1 s2+
Respiratory rate - 22
Cns higher motor functions normal
Speech slurred.
On motor examination,
Hypotonia in left upper limb and lower limb.
Reflexes :
Right. Left
biceps 1+. 1+
Triceps 1+. 1+
Supinator. 1+. 1+
Knee. 1+. 1+
Ankle bilateral absent
Plantar left mute right flexor.
Hand grip : right 100% left 50%
INVESTIGATIONS:
CBP shows increase in luecocytes ( 14,400)
Neutrophils (87) and
decrease in lymphocytes (08).
PCV (37.5) AND MCV (80) are decreased
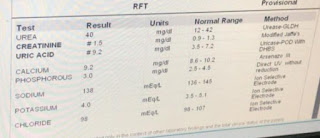
2. RFT shows increase in creatine(1.5) and uric acid levels(9.2).
3. LFT shows increase in alkaline phosphate(139). And total protien count(6.2) is decreased.
4. RBS shows increase in blood glucose(172)
 |
| CHEST X-RAY |
 |
| CT REPORT |
TREATMENT AT HOSPITAL:
Inj. Lorazepam 2cc IV stat (3times).
Inj. Levipil 1gm IV stat.
Inj. NTG 1 amp in 5ml NS.
1ml- @220/110mmhg
1ml- @200/100mmhg(after 3min)
1ml- @140/70mmhg (after 3min)
Inj. Midazolam 4ml IV stat.
Tab. Levipil 500mg BD.
Inj. Lorazepam 2ml IV stat.
BP/PR/spO2 monitoring 2hrly.
Gbrs monitored 6hrly.
Tab. Met-xl 25mg OD.
Tab. Clinidipine 10mg OD.
TREATMENT AT DISCHARGE:
Tab. Levipil 500mg OD.
Tab. Valproate 500mg OD.





Comments
Post a Comment