Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a) The evolution of symptomatology in the patient:
> It begins with shortness of breath more commonly at work rather than at rest. Even the slight amount of pressure/work causes exertion resulting in shortness of breath.
> Gradually, SOB is observed even at resting condition where it is progressed along with pedal edema.
> Bronchiectasis (cough produced with mucus) is observed.
> Then raise in blood pressure/hypertension in the lung arteries is seen.
> Later, the right heart muscle weakens leading to the failure of heart on the right side.
b ) The anatomical localization for the problem is the lung (respiratory system) which later progresses towards the heart.
c ) The primary etiology of patient’s could be because of her occupation where she worked in the paddy fields. Working around the dust arousing from the fields may have caused COPD in the patient.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: a ) Pharmacological interventions:
> Inj AUGUMENTIN 1.2gm IV BO: It is used for treating short term bacterial infection in the case of acute exacerbation of COPD. It contains 2 different medicines that work together to kill the bacteria that cause infections. Amoxycillin works by stopping the growth of bacteria. Clavulanic acid is a beta-lactamase inhibitor that reduces resistance and enhances the activity of amoxicillin against the bacteria.
> TAB. AZITHROMYCIN 500mg OD: Azithromycin kills certain bacteria and reduces inflammation in the lungs, which may help in reducing the number of lung attacks the patient has. It helps in reducing chest symptoms such as coughing, sputum (phlegm) and breathlessness.
> Inj LASIX IV BO: Lasix (furosemide) is an anthranilic acid derivative that is used s strong diuretic to treat excessive fluid accumulation (edema). It is widely prescribed in patients with COPD for the treatment of peripheral edema. It is known that furosemide causes metabolic alkalosis
> TAB PANTOP 40mg PO OD: Used for heatburn and chest pain.
> Inj HYDROCORTISONE 100mg IV: Hydrocortisone is a corticosteroid. It is administered to reduce inflammation. This drug suppresses eosinophils present in the airway which are responsible for inflammation.
> TAB PULMOCLEAR 100mg PO OD: It is a combnation of 2 medicines that helps the airways in the lungs stay open. It works by relxaing the muscles of these airways. This makes it easier for the air to get in and out. It also helps in loosening the thick mucus making easier to cough it out. It will relieve symptoms such as tightening of chest, wheezing, coughing and SOB.
> Inj THIAMINE 1 amp in 100ml of NS: It is effective for treatment of congestive heart diseases and also for the increase in VO2 levels.
b ) Non pharmacological interventions:
Ø HEAD END ELEVATION: It is a commonly used therapeutic intervention in mechanically ventilated patients associated with a reduction in the incidence of ventilator associated pneumonia. It improves oxygenation and hemodynamic performance.
Ø O2 INHALATION: To maintain the spO2 above 92%
Ø INTERMTTENT BiPAP: Bilevel Positive Airway Pressure ventilation is a noninvasive technique used to provide ventilator support to a spontaneously, but insufficiently, breathing patient using a facemask or nasalmask. With this mode of ventilation, BiPAP cycles between two levels of continuous positive airway pressure. This mode of ventilation has resulted in shorter duration of ventilation, less need of sedation and fewer complications. It is useful for the patients with COPD.
CHEST PHYSIOTHERAPY: The Airway Clearance Technique assists in sputum clearance in an attempt to reduce symptoms and paroxysmal coughing, slow the decline in lung function, reduce exacerbation frequency and hasten the recovery from exacerbation.
3) What could be the causes for her current acute exacerbation?
ANS: Recently, her HRTC showed signs of bronchiectasis. [A condition where bronchial tubes of lungs are permanently damaged, widened and thickened. These damaged air passages allow bacteria and mucus to build up and pool in the lungs blocking the airways] This could be a trigger factor for the current acute exacerbation.
4. Could the ATT have affected her symptoms? If so how?
ANS: Yes. Empirical ATT resulted in generalized weakness. A week after ATT, pedal edema and facial puffiness is seen. Some cases of COPD maybe preventable by controlling the TB epidemic, early TB diagnosis and prompt initiation of appropriate anti-TB treatment. Follow-up care and early intervention for COPD maybe necessary for treated TB patients.
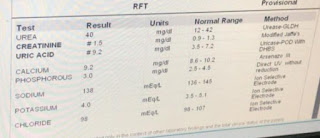
5.What could be the causes for her electrolyte imbalance?
ANS: Patients with COPD are susceptible mainly to hyponatremia (low levels of sodium ions). Chronic hypoxia and hypercapnia secondary to the underlying pulmonary illness, heart failure, use of bronchodilators or steroids, malnutrition during acute exacerbation are common contributing factors for electrolyte imbalance. Activation of Renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may also cause electrolyte imbalance.
2) Neurology (10 Mark)
CASE A] A 40 year old male with complaints of irrelevant talking
Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø 2-3 episodes of seizures, apparently with a gap of 8 months in between.
Ø Alcohol withdrawal symptoms associated with restlessness, sweating and tremors are observed
Ø Sudden onset of talking and laughing to himself was seen.
Ø Disability in lifting himself off the bed move around is seen.
Ø Later, short-term memory loss associated with not being able to recognize family members from time to time was observed.
b ) Anatomical localization include the lower parts of the brain called thalamus and hypothalamus in Wernicke’s encephalopathy.
c ) Primary etiology of the patient’s problem is thiamine deficiency due to excessive alcohol consumption.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: Pharmacological interventions:
Ø IVF NS and RL: Intravenous normal saline is administered as a source for hydration as well as electrolyte balance whereas ringer’s lactate is used to treat dehydration.
Ø Inj THIAMINE 1amp: Thiamine injection is administered as there is a deficiency of thiamine in alcohol addicts.
Ø Inj LORAZEPAM: It is administered in this case to treat seizures of the patient. It binds to a type of GABA receptor and activates it in a similar way to GABA which leads to the inhibition of uncontrolled firing of neurons that causes seizures.
Ø TAB PREGAALIN 75mg/PO/BD: It is an antiepileptic drug. It is also used to treat neuropathic pain. It binds to alpha2-delta subunits and reduces the synaptic release of several neurotransmitters thus preventing the seizure.
Ø LACTULOSE 30ml/PO/BD: It is used in preventing and treating portal-systemic encephalopathy. Its chief mechanism of action is by decreasing the production and absorption of ammonia. It may also be helped in the improvement of mental status.
Ø Inj 2 AMPOULE KCl in 10NS: It is used in the treatment of hypokalemia, prophylaxis for hypokalemia, IV intermittent fusions.
Non pharmacological interventions:
Ø GRBS: General Random Blood Sugar test for detecting blood glucose levels.
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
ANS: Multiple alcohol withdrawals gradually leads to permanent alterations in GABA receptors which causes neurological damage. This is the reason why neurological symptoms appear later than earlier.
4) What is the reason for giving thiamine in this patient?
ANS: Alcohol consumption leads to thiamine deficiency. This is due to poor nutrition causing decrease in essential vitamins. And also alcohol causes inflammation in stomach lining causing reduction in absorption of vitamins.
5) What is the probable reason for kidney injury in this patient?
ANS: Binge drinking alcohol causes high rise of alcohol content in blood causing kidneys to lose their function termed as acute kidney injury. Chronic alcohol abuse results in damage of kidney function leading to the leakage of proteins into the urine, commonly called as Albuminuria which is an early sign of kidney disease.
6). What is the probable cause for the normocytic anemia?
ANS: Heavy alcohol consumption cause generalized suppression of blood cell production and production of structurally abnormal blood cell precursors that cannot fully mature into functional cells. Defective RBCs are destroyed prematurely causing low number production of them resulting in normocytic anemia.
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
ANS: Chronic alcoholism can cause nutritional deficiencies and alcohol toxicity. These can inturn cause poor wound healing and problems with nerves (neuropathy). When sensory nerves in foot stop working, the foot can get injured and this leads to foot ulcers.
CASE B] A 52 year old male with cerebellar ataxia.
Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø The beginning symptom was giddiness which briefly subsided after rest.
Ø Giddiness was associated with vomiting on the same day
Ø After being asymptomatic for 3 days, sudden onset of giddiness appeared again which was progressive in severity while walking.
Ø Bilateral hearing loss, aural fullness and presence of tinnitus were seen.
Ø Association of 2-3 episodes of vomiting per day which were non projectile, non bilious containing food particles was observed.
Ø H/o postural instability (unable to walk without support), tendency to fall while walking and swaying is present.
b ) Damage to unilateral cerebellar hemisphere causes ipsilateral cerebellar ataxia.
c ) primary etiology of the patient’s problem is due to excessive consumption of alcohol.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: Pharmacological interventions:
Ø TAB VERTIN 8mg PO TID: It is used to treat hearing loss as bilateral hearing loss is seen in the patient. It is a betahistin which improves the microcirculation of the inner ear. It works as antagonist of H3 receptors against which it has a strong effect.
Ø Inj ZOFER 4mg IV/TID: It is used to prevent and manage nausea and vomiting.
Ø TAB ATORVOSTATIN 40mg PO/HS & TAB ECOSPRIN 5mg: Both of these drugs are administered to prevent heart attacks and heart strokes as the patient past history shows denovo hypertension.
Ø TAB MVT & THIAMINE 1amp in 100ml NSPO/BD: Multivitamins and thiamine are administered as a source for essential vitamins as the patient is alcoholic.
Non pharmacological interventions:
Ø BP MONITORING: Since the patient is hypertensive, BP is monitored frequently.
3) Did the patients history of denovo HTN contribute to his current condition?
ANS: Yes, patient’s history of denovo HTN contributes to his current condition of CVA. The etra strain that high BP puts on the blood vessels may cause a weakened blood vessel to burst inside the brain, causing bleeding on and into surrounding tissues. This is called a hemorrhagic stroke which is a type of cerebrovascular accident.
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
ANS: Patient’s alcoholism causes hemorrhagic stroke. That is because liver damage due to too much alcohol can stop liver from making substances which are responsible for blood clot. This causes the risk of having a stroke caused by bleeding in the brain which is called as hemorrhagic stroke
CASE C] A 45 years old female patient with palpitations, pedal edema and radiating pain along upper limb.
Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø Development of bilateral pedal edema with a gradual progression present in both sitting and standing positions.
Ø Sudden onset of palpitations, more during the night, are seen after 8 months of development of bilateral pedal edema.
Ø Aggravation of palpitations occurred during weight lifting and continuous speaking along with dyspnoea.
Ø Radiating pain from chest in the upper limb is observed along with chest heaviness
b ) Anatomical localization for the patient’s problem of Cervical spondylosis include intervertebral discs present between cervical vertebrae. And that of recurrent hypokalemic paralysis include muscles of arms and legs.
c ) Dehydrated disks due to aging, generally by the age of 40, causes drying out and shrinking of spinal disks which allows more bone-on-bone contact between the vertebrae resulting in cervical osteoarthritis (spondylosis). As the patient’s age is 45, aging can be considered as the primary etiology.
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
ANS:The patient complained of sudden onset of aggravating palpitations. She was relieved on using medication. Diuretics (water pills) are administered for irregular heartbeat. Use of diuretics cause loss of water along with sodium and potassium ions resulting in hypokalemia.
Important risk factors for her hypokalemia include medications like diuretics which are being administered for palpitations.
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
ANS: ECG changes include flattening and inversion of T waves in mild hypokalemia, followed by Q-T interval prolongation, visible U wave and mild ST depression in more severe hypokalemia.
Associated symptoms included in severe hypokalemia can result in arrhythmias and ventricular tachycardia.
CASE D] A 55 year old patient with seizures.
Link to patient details:
QUESTIONS:
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
ANS: Yes, there is a relation between occurrence of seizure and brain stroke. The mechanism involved is as follows: A stroke causes the brain to become injured. The injury to brain results in the formation of scar tissue which affects the electrical activity in brain. Disrupting the electrical activity can cause the occurrence of a seizure.
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
ANS: In the recent episode, the seizure was tonic-clonic which is a grand mal seizure. Grand mal seizure causes a loss of consciousness and violet muscle contractions. It is caused by abnormal electrical activity throughout the brain. Previous episodes of seizures did not show tonic-clonic movements.
CASE E] A 48 year old male with seizures and altered sensorium.
Link to patient details:
Questions: 1) What could have been the reason for this patient to develop ataxia in the past 1 year?
ANS The reason for ataxia in the patient maybe due to head trauma, where he reportedly mentioned about several falls on head which were left unattended. It could also be due to the alcohol intoxication as the patient is an addict since 3 years.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
ANS: Binge drinking alcohol causes low affinity of hemoglobin binding to oxygen leading to low levels of oxygen saturation. Deprived oxygen to the brain can cause Intracranial hemorrhage (ICH). As the patient was binge drinking alcohol 3hrs prior to the drowsiness, this could have been the reason for his IC bleed.
Yes ,chronic alcoholism contributes to bleeding diathesis associated with impaired platelet function together with reduced platelet count.
CASE F] A 30 year old male patient with weakness of right upper limb and left lower limb.
Link to patient details:
Questions
1.Does the patient's history of road traffic accident have any role in his present condition?
ANS: Yes, there may be role in the present condition in which there is nerve injury and progressive degeneration which results in the present condition of the patient.
2.What are warning signs of CVA?
ANS: sudden numbness or weakness in arm or leg especially on one side of body; Sudden confusion, trouble speaking; Sudden trouble walking, dizziness, loss of balance and coordination.
3.What is the drug rationale in CVA?
ANS: a ) Oxygenation: Maintaining adequate tissue oxygenation is important during acute CVA in order to prevent hypoxia.
b) Antihypertensives: In CVA, many patients will have elevated BP for first 24-48hrs. Inorder to prevent relative hypertension, lowering the blood pressure should be done cautiously
4. Does alcohol has any role in his attack?
ANS: Two or more drinks per day increases the risk of causing a stroke. But the patient consumed alcohol once in a week. So there are less chances of role of alcohol in his attack.
5.Does his lipid profile has any role for his attack??
ANS: His lipid profile is normal. Hence, doesn’t have any role in his attack.
CASE G] A 50 year old patient with cervical myelopathy.
Link to patient details:
__*Questions*_
1)What is myelopathy hand ?
ANS: There is loss of power of adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers. These changes have been termed "myelopathy hand" and appear to be due to pyramidal tract involvement.
2)What is finger escape ?
ANS: Finger escape
Wartenberg's sign is a neurological sign consisting of involuntary abduction of the fifth (little) finger, caused by unopposed action of the extensor digiti minimi. . This finding of weak finger adduction in cervical myelopathy is also called the "finger escape sign".
3)What is Hoffman’s reflex?
ANS: Hoffman's sign or reflex is a test used to examine the reflexes of the upper extremities. This test is a quick, equipment-free way to test for the possible existence of spinal cord compression from a lesion on the spinal cord or another underlying nerve condition
CASE H] A 17 year old female with seizures.
Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
ANS: Iron deficiency anemia is seen in the patient. Cortical venous thrombosis is often caused due to iron deficiency. Seizures are the presenting feature of cortical venous thrombosis. This can be the cause of her condition.
2) What are the risk factors for cortical vein thrombosis?
ANS: Risk factors include Sickle cell anemia, Chronic hemolytic anemia, Problems with blood clots, low blood pressure in the brain (intracranial hypotension). Etc..
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
ANS: The antiepileptic drugs were tapered off after a 3-day seizure free period in the patient. Sometimes, withdrawal of the antiepileptic drugs cause seizures in some patients. The sudden episode of GTCS was resolved spontaneously because if there is a single episode of grand mal seizure, it may have been an isolated event and doesn’t usually require treatment.
4) What drug was used in suspicion of cortical venous sinus thrombosis?
ANS: Injection Clexane 0.4ml s/c BD was used in suspicion of cortical venous thrombosis as it is used to treat blood clots.
3) Cardiology (10 Marks)
CASE A] A 70 year old male with shortness of breath, chest pain, B/L pedal edema and facial puffiness.
Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
ANS: Preserved ejection fraction (HFpEF) is also referred as diastolic heart failure. The heart muscle contracts normally but the ventricles do not relax as they should during ventricular filling.
Reduced ejection fraction (HFrEF) is also referred as systolic heart failure. The heart muscle does not contract effectively, and therefore oxygen rich blood is supplied to the body.
2.Why haven't we done pericardiocenetis in this pateint?
ANS: An invasive procedure like peri-cardiocentesis is only indicated when the effusion is large or symptomatic and the effusion is accompanied by tamponade. This patient has moderate pericardial effusion and also there is no presence of tamponade and hence pericardiocentesis is not done.
3.What are the risk factors for development of heart failure in the patient?
ANS: The major risk factors associated with poor prognosis in acute pericarditis include high ffever, subacute course, evidence of large pericardial effusion, cardiac tamponade and dailure to respond with seven days to non steroidal anti-inflammatory drugs (NSAIDs). And also as the person is a chronic smoker and drinker, the risk of heart failure increases if he does not reduce the alcohol intake and quit smoking.
4.What could be the cause for hypotension in this patient?
ANS: In acute pericarditis, some patients show swelling of ankles (bilateral pedal edema in case of this patient) and low blood pressure resulting in hypotension.
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
ANS: The patient has been diagnosed with type 2 diabetes mellitus which is a high risk factor for heart failure. Additionally he is also suffering from diabetic triopathy where diabetic nephropathy can cause heart failure. The patient also has hypertension and a chronic drinker which could also have been the possible factors for his heart failure.
2.what is the reason for anaemia in this case?
ANS: As the patient is diagnosed with diabetic nephropathy, there will be reduced production of erythropoietin by the kidneys. This results in anemia of chronic disease in the patient.
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
ANS: The reason for formation of blebs on his feet is due to diabetes mellitus. Blisters typically occur in people whose sugar levels are not in control.
People with diabetes have problems with immune system activation. This often causes poor wound healing in diabetic patients. This is the reason for his non healing ulcers in the legs.
4. What sequence of stages of diabetes has been noted in this patient?
ANS: Type 2 diabetes mellitus which is followed by diabetic retinopathy and which later progressed to cause diabetic nephropathy and which can lead to eloctolytic changes and which may aslo casue multiorgan failure in uncontrolled stages.
CASE C] A-Fib and Biatrial Thrombus in a 52yr old male.
Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø On and off pain at inguinal surgical site since 3 years.
Ø Facial puffiness on and off since 2-3yrs.
Ø Hypertension since 1yr.
Ø Grade-2 shortness of breath since 1 year.
Ø Progression of SOB to grade-4.
Ø Decreased urine output and anuria since 2 days.
b ) Anatomical localization in atrial fibrillation includes the upper chambers of heart, the atria, beat irregularly (quiver) instead of beating effectively to move blood into the ventricles.
c ) Hypertension in the patient is the primary cause of atrial fibrillation.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: Pharmacological interventions:
Ø Inj DOBUTAMINE 3-6ml/hr: Used to treat cardiogenic shock and severe heart failure. It acts on alpha-1, beta-1 and beta-2 adrenergic receptors. In the heart, the stimulations of these receptors produces a relatively strong, additive inotropic effect and a weak chronotropic effect.
Ø TAB DIGOXIN 0.25mg: Used for the treatment of heart failure. It helps to provide symptomatic relief by making heart pump blood more efficiently.
Ø Inj UNFRACTIONATED HEPARIN 5000 IU TID: Used as an anticoagulant (blood thinner). It produces anticoagulant effect by inactivating thrombin and activated factor-X through an antithrombin dependent mechanism. It not only prevents fibrin formation but also inhibits thrombin-induced activation of platelets and of factors V & VIII.
Ø TAB CARVEDILOL 3.125mg BD: Used to treat hypertension and heart failure. It works by blocking the action of certain natural substances in body such as epinephrine, on the heart and blood vessels. This effect lowers the heart rate and BP.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
ANS: Atrial fibrillation or heart failure can both cause the development of chronic kidney disease (CKD) which is diagnosed in the patient. This is the result of activation of the sympathetic nervous system, the renin-angiotensin-aldosterone-system (RAAS), and mediators of inflammation and fibrosis. Type 2 CRS which is the chronic CRS is present in this patient.
4) What are the risk factors for atherosclerosis in this patient?
ANS: Risk factor for atherosclerosis in this patient is hypertension and which can also causes caridac disorders like MI or any plaque rupture causes heart attack and blockage of coronary arteries which results in ischemia.
5) Why was the patient asked to get those APTT, INR tests for review?
ANS: Biatrial thrombus is a well-known complication of atrial fibrillation which the patient is suffering from and it carries a high risk of thromboembolism. APTT test measures the length of the time (in seconds) that is taken for the clotting to occur and evaluates coagulation factors. INR test measures the time for blood to clot. It is also known as prothrombin time.
CASE D] A 67 year old patient with acute coronary syndrome.
Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø DM2 since 12 years.
Ø History of pulmonary TB 7 months ago.
Ø Heartburn episodes since a year
Ø Hypertension since 6 months.
Ø Shortness of breath and sweating on exertion on the day of visit to OPD.
b ) Anatomical localization includes the heart musculature.
c ) Primary etiology of the patient’s problem of acute coronary symptom is Diabetes mellitus type 2 which his apparently a high risk factor for ACS. Additionally, patient’s age and hypertension could have factored to it.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
Ø TAB MET XL 25mg/STAT: It is used to reduce high blood pressure mainly, along with conditions like chest pain and heart failure. It works by relaxing the blood vessels, slowing down the heart rate. By doing this, it reduces workload on the heart of pumping the blood effectively.
3) What are the indications and contraindications for PCI?
ANS: a ) INDICATIONS:
Ø Acute ST-elevation myocardial infarction (STEMI).
Ø Non ST-elevation acute coronary syndrome (NTSE-ACS).
Ø Unstable angina.
Ø Stable angina.
Ø Anginal equivalent (Eg: Dyspnea, Arrhythmia, Dizziness or Syncope).
Ø High risk stress test findings.
b ) CONTRAINDICATIONS:
Ø Intolerance for oral antiplatelets long term.
Ø Absence of cardiac surgery backup.
Ø Hypercoagulable state
Ø High grade chronic kidney disease.
Ø Chronic total occlusion of SVG
Ø An artery with a diameter of <1-5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
ANS PCI shouldn’t be performed in this patient as it is not safe to use PCI in the person having blocked arteries. If a PCI is performed in a patient who doesn’t need it, complications arise. The most possible complication is that, artery blockage returns to scar tissue (restenosis).
The harms of over-treatment arise from situations where normal life experiences are deemed illnesses or when diseases are “created” from mild problems and symptoms. In both situations, people become patients and their problems are deemed to need medical treatment when they may not need it or could be harmed by it.
The potential harms of over-testing arise through misdiagnosis, false positive results, false negative results and over-diagnosis, where people are labeled as having a “disease” for a condition that would not have caused them harm if it were left undetected and untreated.
This is why research on overtreatment and over-testing important to current healthcare system.
CASE E] A 60 year old male patient with chest pain, giddiness and profuse sweating.
Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø Known case of hypertension and diabetes mellitus type 2.
Ø Mild chest pain in the right side of chest.
Ø Dizziness was developed.
Ø Profuse sweating was observed.
b) Anatomical localization includes occlusion or right coronary artery on the inferior wall of the heart.
c) Primary etiology is the type 2 diabetes mellitus seen in the patient along with hypertension.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
ANS: Pharmacological interventions:
Ø TAB ASPIRIN 325mg: It is used as a pain killer given for chest pain.
Ø TAB ATORVAS 80mg: It lowers the bad cholesterol and triglycerides and increases good cholesterol.
TAB CLOPIBB 300mg: Used to prevent blood clot formation in hardened blood vessels thus reducing risk of heart attack, stroke and heart related chest pain
CASE F] A case of cardiogenic shock.
Link to patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
ANS: Because of the fluid loss occurred to the patient there is decreased preload- so, SOB occurred due to decreased CO
IV fluids administered- there is increased preload- SOB decreased due to better of cardiac output.
2. What is the rationale of using torsemide in this patient?
ANS: Torsemide used to relieve abdominal distension.
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
ANS: IT IS THE TREATMENT FOR UTI
Rationale- Used for any bacterial infection.
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø Painabdomen & Vomitngs 5yrs ago.
Ø Repetition of symptoms 3yrs ago.
Ø 5-6 episodes of the same symptoms in the past 1yr.
Ø Fever from 4 days.
Ø Throbbing pain in abdomen which started radiating back associated with nausea and vomiting
Ø High grade fever
Ø Development of constipation and burning micturition associated with suprapubic pain.
b ) Anatomical localization include acute inflammation of pancreas, accompanied by abdominal pain. This syndrome is usually a discrete episode, which may cause varying degress of pain to the pancreas and adjacent & distant organs.
c ) Primary etiology of acute pancreatitis in this patient is excessive consumption of alcohol.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS: Pharmacological interventions:
Ø Inj MEROPENAM: It is used to treat skin and abdominal infections.
Ø Inj METROGYL: It is also used to treat variety of infections and prevents the growth of bacteria.
Ø Inj AMIKACIN: Used to treat infections of blood, abdomen, lungs, skin, bones, joints and urinary tract.
Ø Inj OCTREOTIDE: It is an inhibitor of exocrine secretion of pancreas, which plays an important role in acute pancreatitis.
Ø Inj TRAMADOL: It is a potent analgesic used in severe pancreatitis pain.
CASE B] A 25 year old man with epigastric pain.
Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
ANS: Acute pancreatitis causes secretion of a lot of inflammatory chemicals into the blood stream, including the lungs. This affects the lung function, causing the level of oxygen in the blood to dangerously low levels resulting in shortness of breath/dyspnea.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
ANS: Pancreatitis causes diabetes by affecting the amount of insulin production. As a result, diabetes as a consequence may require insulin injections. This could have been the reason why the patient has developed a state of hyperglycemia.
Acute Pancreatitis
↓
Damage to the Pancreatic
Beta cells
↓
Decreased Synthesis and release
of Insulin
↓
Increased Glucagon stores
↓
Hyperglycemia
3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
ANS: In general, the reasons for elevated LFTs include metabolic syndrome; hepatitis; alcohol use disorder and cirrhosis. As this patient has alcohol addiction, this could have been the reason for his elevated LFTs. Specific markers for Alcoholic Fatty Liver disease include elevated alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels.
4) What is the line of treatment in this patient?
For the master chart to the "pancreatitis thesis project" please get in touch with Dr Shashikala PGY1 and Dr Divya PGY2 and share their insights into the above project problem they are working on.
ANS: Line of treatment strategies for acute pancreatitis include fasting and short-term intravenous feeding, fluid therapy and pain management with narcotics for severe pain or nonsteroidal anti-inflammatories for milder cases.
C) Link to patient details:
Possible Questions :-
1) what is the most probable diagnosis in this patient?
ANS: The probable diagnosis of the patient is might be liver abscess , hepatomegaly.
2) What was the cause of her death?
ANS:As per patient's history, the next day of surgery Patient had suffered with severe cough and Shortness of breath eventually resulting in Abnormalities in Vital signs. So, Sepsis or Acute respiratory distress syndrome might be the cause of the death in this patient.
3) Does her NSAID abuse have something to do with her condition? How?
ANS: Patient's USG report reveals that She had Grade 3 RPD changes of Right kidney.
It highly suggests that she may had underlying CKD (Chronic Kidney Disease)
Which is secondary to her chronic usage of NSAIDS.It is so called Analgesic Nephropathy.
5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
1. What could be the reason for his SOB ?
ANS: Reason for his sob can be POST TURP SYNDROME: it occurs because of irrigation of absorption of large volumes of irrigation fluid during turp which can cause HYPONATREMIA,CARDIORESPIRATORY depression.
2. Why does he have intermittent episodes of drowsiness ?
ANS: The hyponatremia which occurs as a part of post turp syndrome :low levels of sodium in the body can cause lethargy,fatigue and sleep. that cause drowsiness.
3. Why did he complaint of fleshy mass like passage in his urine?
ANS: Passing of fleshy like mass which is foamy can be because of infection where pus cells are more. like in the case of urinary tract infections.
4. What are the complications of TURP that he may have had?
ANS: complications of turp can be bladder injury,bleeding,hematuria,dysuria,infection. in this patient it can be infection as pus cells are seen .
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
ANS: The child is excessively hyperactive without much of social etiquette because of Attention-Deficit/Hyperactivity Disorder which has been diagnosed recently.
2. Why doesn't the child have the excessive urge of urination at night time ?
ANS: The child doesn’t urinate when asleep because there can be a chance of the manifestation being psychosomatic or as a result of an anxiety disorder or a stress triggering this manifestation.
3. How would you want to manage the patient to relieve him of his symptoms?
ANS: The symptoms can be reduced by various sources which include medication like non-stimulants; psychotherapy & psychosocial interventions; education or training; or a combination of treatments
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
CASE A] A 40yr old lady with Dysphagia, Fever and Cough.
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
ANS: The physical findings indicative of TEF are Cough, Hoarseness of voice and Difficulty in swallowing both solids and liquids.
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
ANS: In this case, the patient was diagnosed with RVD and since then she started on ART. Patients with mycobacterial and cryptococcal disease at the time of initiation of ART are at higher risk of developing Immune Reconstitution Inflammatory Syndrome with an approximate risk of 15%. Patients with TB (as in the case of this patient) are at higher risk of developing IRIS.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?What could be the cause in this patient ?
ANS: yes, it could be due to intake of contaminated toddy.
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
ANS: According to some studies, alcoholism mainly consuming locally prepared alcohol plays a major role as a predisposing factor for the formation of liver abscesses that is for causation of both amoebic as well as pyogenic liver abscess because of the adverse effects of alcohol over the Liver which damages it in many different ways.
3. Is liver abscess more common in right lobe ?
ANS: yes right lobe is involved due to its more blood supply , As increase in blood supply increase intransportation of inflammaotory substances which increase in inflammation and formation of abscess.
4.What are the indications for ultrasound guided aspiration of liver abscess ?
ANS: Indications for USG guided aspiration of liver abscess
- amoebic liver abscess
-Large abscess more than 6cms
- Left lobe abscess
-Caudate lobe abscess
-. Abscess which is not responding to drugs
-seronegative abscess
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
ANS: As patient history suggests he is occasionsal toddy drinker , any contamination can cause liver injury, and also he is on high dose of antibiotics and pain killers which has a chance of damage to liver and kidney.
2) How do you approach this patient ?
ANS: *Based on right hypochondriac and epigastric pain , fever
* USG finding of hyperechoic mass in right lobe of liver along with other supportive investigations like leucocytosis ( suggestive of infection/inflammation) and ALP ( Alkaline phosphatase ) rise in LFT is a suggestive diagnosis of LIVER ABCESS.
3) Why do we treat here ; both amoebic and pyogenic liver abcess?
ANS: • Considering the risk factors associated with the aspiration of pus for culture like :-
1) Some times abscess is not accessible for aspiration if it is in posterior aspect.
2) Sometimes it has thinwall which may
rupture if you try to aspirate resulting in complications.
3) Sometimes it is unliquified.
• For this reason, we treat both PLA and ALA emperically in clinical practice.
• PLA and ALA have many features in common and diagnosis is often delayed due to vague clinical symptoms resulting in adverse
outcomes.
• Because of the difficulty in differentiating
between these two types of abscesses initially, antiamoebic therapy is usually recommended in addition to broad-spectrum antibiotics.
• Medical therapy alone is effective in most cases of ALA .
• While some form of intervention is usually needed for PLA.
• Mortality is low with ALA compared with PLA.
4) Is there a way to confirmthe definitive diagnosis in this patient?
ANS: On Analysis of Laboratory Reports and the findings that suggests the diagnosis of Liver abscess are :-
• Symptomatology of Right Hypochondriac and Epigastric pain, Fever with chills and rigors
• Hematological findings like Leukocytosis (Indicates Infection/Inflammation) and
Anaemia
• Biochemical findings like Elevated levels of Alkaline Phosphatase and Hypoalbuminemia
in LFT
• USG finding of Hyperechoic mass in the Right lobe of the liver
Considering the following factors like:-
• Age of the Patient which is 21
• Gender - Male
• Solitary abscess
• Location of abscess which is Segment 8 in the right lobe
*The abscess is most likely to be Amoebic Liver abscess.
This can definitively be confirmed by :-
* Microscopic stool examination is still of little value if the serological and antigen detection tests are not available.
* Stool antigen detection based on Enzyme immunoassay are most common and quite sensitive which facilitates early diagnosis before the antibody response occurs (< 7d) compared to the PCR based methods which is not well standardized and is not widely available.
* Stool culture for amoeba is sensitive but has limited availability.
* Serologic testing is the most widely used method of diagnosis for amebic liver abscess. In general, the test result should be positive, even in cases when the result of the stool test is negative (only extra-intestinal disease).
- EIA has now largely replaced indirect hemagglutination (IHA) testing and counter immunoelectrophoresis (CIE) testing which is relatively simple and easy to perform, rapid, inexpensive, and more sensitive which detects antibodies specific for E histolytica in approximately 95% of patients with extra-intestinal amebiasis.
- Entamoeba histolytica galactose lectin antigen is detectable by enzyme-linked immunosorbent assay (ELISA) in at least 75% of serum samples obtained from patients with amebic liver abscess.This test can be used for rapid diagnosis in highly endemic areas, where serology can be misleading, but it is not widely available.
* Aspiration may be performed under computed tomography (CT) scan or sonographic guidance.
• Send the collected specimen for Gram stain and cultures.
• Amoeba rarely are recovered from the aspirate (15%) and, often, they are present only in the peripheral parts of the abscess, invading and destroying adjacent tissue.
• Amoebic liver abscesses only rarely yield positive bacterial cultures following secondary bacterial infection of the abscess cavity.
• Detecting E histolytica antigen in the aspirate is possible and is accomplished as previously described for stool specimens. It is highly specific. The sensitivity was only 20% using enzyme-linked immunosorbent assay (ELISA), but newer polymerase chain reaction (PCR)-based assays have a sensitivity of 83% and a specificity of 100%. [28, 29] However, currently, PCR-based detection is not widely available.
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
ANS: a ) Evolution of symptomatology:
Ø Hypertension since 3yrs.
Ø Fever associated with chills and rigors.
Ø Generalized weakness, facial puffiness and preorbital edema along with drowsiness.
Ø Weakness of upper and lowerlimbs
Ø Diagnosis of Diabetic ketoacidosis.
b ) Anatomical localization include nasal or palatine findings of mucormycosis including grey or reddish mucosa which will progress to black areas of eschar as necross ensues. Eschar maybe seen in nasal septum, palate, eyelid, face, or orbital areas.
c ) Primary etiology of the Rhino-orbital mucormycosis is generally diabetes from which the patient is suffering in this case.
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
ANS: 1) Pharmacological interventions:
Ø Inj. LIPOSOMAL AMPHOTERICIN B: It is used to treat fungal infections. It binds to ergosterol in the fungal cell membrane, which leads to formation of pores, ion leakage and ultimately fungal cell death.
Ø ITRACONAZOLE 200mg: It is also used to treat fungal infections. It acts by inhibiting the fungal cytochrome P-450 dependent enzyme lanosterol 14-alpha-demethylase. When this enzyme is inhibited it blocks the conversion of lanosterol to ergosterol, which disrupts fungal cell membrane synthesis.
Ø DEOXYCHOLATE AMP B: It is used as a fungicidal. Polyenes bind to ergosterol in the fungal cell wall, disrupting the cell, altering its permeability and killing the fungus.
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
ANS: People with more severe forms of COVID-19 are treated with steroid medications, whch can suppress the immune system, opening them up to a fungal infection like mucormycosis.
And also, people who do not maintain hygiene with masks are also being affected with mucormycosis as the unhygienic masks develop moisture which is leading to this condition at this point of time.
9) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
1) Covid 19 with co morbidity (Pulmonology/Rheumatology)
Possible questions:
1) How does the pre-existing ILD determine the prognosis of this patient?
ANS:In patients with preexisting ILD, COVID-19 infection has led to acute exacerbation of underlying ILD. The criteria for ILD exacerbation include subacute worsening of dyspnea and hypoxemia, new pulmonary infiltrates on imaging, and absence of pulmonary emboli, cardiac failure, and other non-pulmonary causes.
2) Given the history of autoimmune disease in the patient, how does the administration of steroids for COVID affect her RA and hypothyroidism?
ANS: The administration of steroids for COVID affects in a rapid and sustained decrease in RA disease activity. Whereas, it has an inhibitory effect on TSH secretion at the pituitary level which does not help in case of hypothyroidism.
3) Why was she prescribed clexane (enoxaparin)?
ANS: Clexane beng a blood thinner is given to her because the Erythrocyte Sedimentation Rate (ESR) is high in the patient.And it is also given as in covid patients there is chance of blood clots due to damege of endothelial cells and activaton of clotting mechanism. To suppress blood thinners are given.
2) Covid 19 with Diabetes
Link to the patient case report log:
Questions:
1) Since patient didn't show any previous characteristic diabetes signs, did the Covid-19 infection aggravate any underlying condition and cause the indolent diabetes to express itself? If so what could be the biochemical pathways that make it plausible?
ANS: Covid-19 is not the reason behind aggravation of underlying diabetes. The diabetes was found out accidentally when she came to visit the hospital.
2) Did the patient's diabetic condition influence the progression of her pneumonia?
ANS: Yes, diabetes causes poor healing process of inflammation in lungs. The increase in the blood glucose levels helps the growth of virus and this results in rapid progression of pneumonia n the patient. It also affects the immune system of body and weakens it. Hence diabetes is considered as a risk factor in COVID patients.
3) What is the role of D Dimer in the monitoring of covid? Does it change management or would be considered overtesting?
ANS: Amid the COVID-19 pandemic, elevated D-dimer levels have been associated with disease severity and mortality trends. There seems to be no consensus yet as to how D-dimer levels should be used for monitoring COVID-19 patients. Checking D-dimer on initial presentation in the ER is appropriate. Based on available COVID-19 experience on D-dimer testing, there seemed to have a higher risk of poor outcomes. So in a way, this could be considered an overtesting.
3) Covid 19 Severe
Link to the complete case report log:
Questions:
1. Why was this patient given noradrenaline?
ANS: Nor adrenaline being a vasoconstirctor, as the patient had sudden hypotension to treat it they have prescribed noradrenaline which increase the blood pressure.
2. What is the reason behind testing for LDH levels in this patient?
ANS: As increase in LDH shows there is some amount of tissue damage , hence the level of LDH are being tested. If there is increase in LDH levels, it denotes ther is inflammation gooin on, and if there is very drastic increase in levels show there is multi organ failure in this patient.
3. What is the reason for switching from BiPAP to mechanical ventilation with intubation in this patient? What advantages did it provide?
ANS: BiPAP is nothing but a non invasive therapy which sends a positive pressure and help the patient to respire in conditions of decreased oxygen saturation, but in this patient ther is drop of oxygen saturation to 30% . So, BiPAP is not useful in this situation. So, they have started intubating which pushes the air directly in the lungs without any patients support. Hence intubation was preferred in this case.
4) Covid 19 Mild
Link to the case report log:
Questions:
1. Is the elevated esr due to covid related inflammation?
ANS: It is speculated that COVID-19 might trigger the change of the form of erythrocytes or plasma characteristics including the immune system via an unknown mechanism to increase the ESR. So there are chances that the elevated ESR is due to COVID related inflammation.
2. What was the reason for this patient's admission with mild covid? What are the challenges in home isolation and harms of hospitalization?
ANS: Challenges faced by COVID patients in self isolation include:
Ø Physical challenges like staying in constant touch with medical professionals.
Ø Underlying challenges faced by people with small homes to isolate themselves away from other family members.
Ø Challenges faced by elders to have an oxygen cylinder handy.
Ø Mental stress of having other family members infected.
5) Covid 19 and comorbidity (Altered sensorium, azotemia, hypokalemia)
Link to the case report log:
Questions:
1) What was the reason for coma in this patient?
ANS: The patient is a chronic smoker and drinker as per the reports. It is seen that tobacco users face a greater risk of progression of COVID infection as their lung health is already compromised. The common causes of coma include oxygen deprivation and consumption of toxins. As COVID causes oxygen deprivation and also the patient consumes alcohol, these could’ve been the reasons for coma in this patient.
2) How may covid 19 cause coma?
ANS: COVID-19 causes oxygen deprivation. Deprivation of oxygen to brain is one of the major cause for coma. This way, patients with COVID are often being comatosed.
6) Severe Covid 19 with altered sensorium
Link to the case report log:
1. What was the cause of his altered sensorium?
ANS: In this patient being the chronic alcoholic , after admission to hospital there is withdwral of alcohol. The withdrawl of alcohol suddenly whch causes altered mental status.
2. What was the cause of death in this patient?
ANS: Cardio pulmonary areest might be the cause of death in this patient
7) Covid 19 Moderate with ICU psychosis
Link to the case report log:
Questions :
1)What is the ideal day to start steroids in a patient with mild elevated serum markers for COVID ?
ANS: If the oxygen saturation falls below 94% with complications in lung & throat, persistent high fever for a week, then steroids might be prescribed. But the body should be given opportunity to fight the infection during the first 4-5 days of the disease. Hence, the ideal time to administer steroids would be after 5 days of infection.
2)What all could be the factors that led to psychosis in her ?
ANS: In case of COVID, it is believed that the cause of psychosis could be linked to the severe inflammatory response and vascular changes. Neurotoxins released during this inflammatory response could be contributing to the development of psychosis
3)In what ways shall the two drugs prescribed to her for psychosis help ?
ANS: Resperidone is a second generation antipsychotic (SGA) or atypical antipsychotic. It rebalances dopamine and serotonin to improve thinking, mood and behavior.
Piracetam is most commonly used for breath-holding attacks and for a movement disorder often caused by antipsychotic drugs.
4)What all are the other means to manage such a case of psychosis?
ANS: Other than antipsychotic drugs, psychotherapy also helps to treat cognitive issues and other symptoms of psychosis.
5)What all should the patient and their attendants be careful about ( w.r.t. COVID )after the patient is discharged ?
ANS: Post COVID stuff to be taken care of include:
Ø Daily check of oxygen saturation.
Ø Watch for persistence of respiratory symptoms.
Ø Persistent raise of body temperature.
Ø Regular blood pressure monitoring.
Ø A proper post discharge rehabilitation plan for patient with psychological stress and disorders.
8) Covid 19 Moderate
Link to the complete case report log
Questions:
1. Can psoriasis be a risk factor for severe form of COVID?
ANS: According to a few reports, if a person is taking an immunosuppressive medication for psoriasis, that may increase the risk of contracting COVID-19 relative to the rest of the population. However, the details behind this are not clearly known.
2. Can the increased use of immunomodulatory therapies cause further complications in the survivors?
ANS: Increased use of immunomodulators, including biologic agents represent a potentially vulnerable population during the COVID-19 pandemic and cause further complications in the survivors.
3. Is mechanical ventilation a risk factor for worsened fibroproliferative response in COVID survivors?
ANS: Increasing evidence from experimental and clinical studies suggests that mechanical ventilation, which is necessary for life support in patients with severe COVID can cause lung fibrosis, which may significantly contribute to morbidity and mortality.
9) Covid with de novo Diabetes
Link to Case report log:
•What is the type of DM the patient has developed ?(is it the incidental finding of type 2 DM or virus induced type 1DM )?
ANS: It is most probably the type -1 diabetes ,developed due to viral infection and cytokine storm induced damage to pancreas might have caused the diabetes .!so it could be virus induced type -1 DM .
•Could it be steroid induced Diabetes in this patient?
ANS: There is a chance for steroid induced diabetes too but it doesn’t seem much significant when compared to virus induced diabetes .
10) Comparing two covid patients with variable recovery
What are the known factors driving early recovery in covid?
*On comparing CT images,it is observed that-there is marked crazy paving peripherally in patient.1 .Whereas in patient .2 it is not appreciated .Suggesting severe inflammatory reaction in patient.1 So, there is speedy recovery in patient 2.
*Whereas in patient.2 prolonged fever and new onset diabetes were absent ,and many other factors would have favoured her early recovery .
*People who have delayed recovery are of the opinion that the treatment is not appropriate and blame the treatment process, but there are several other factors that are responsible for clinicaloutcome of a disease .We need to pay special attention in terms of progression of disease and factors effecting the disease process .
11) Covid moderate with first time detected diabetes:
Link to Case report log :
Questions-
1) How is the diabetes related to the prognosis of COVID patients? What are the factors precipitating diabetes in a patient developing both covid as well as Diabetes for the first time?
ANS: Diabetes causes poor healing process of inflammation in lungs. High blood glucose levels effects the immune system and does not help in the prognosis of COVID in patients with diabetes.
2) Why couldn't the treating team start her on oral hypoglycemics earlier?
12) Moderate to severe covid with prolonged hospital stay:
Questions :-
1) What are the potential bioclinical markers in this patient that may have predicted the prolonged course of her illness?
ANS: Potential biochemical markers include:
Ø Elevated levels of overall level of serum CRP.
Ø Elevated levels of LDH.
13) Severe covid with first diabetes
Link to Case report log :
1)What are the consequences of uncontrolled hyperglycemia in covid patients?
ANS: In uncontrolled hyperglycemia which can be a rsk factor for the progression of covid in covid factor in which it causes damage to kidney which makes the condition of the patient more worse.So, there sholud be careful observation of GBRS for evry 6hrly and any other comorbidities like hypertension which deprive the condition.
2)Does the significant rise in LDH suggests multiple organ failure?
ANS: LDH values elevates in any type of inflamation, if there is slight increase in LDH , it says there is a infection or inflammation going on. If there is a sudden rise in the levels of LDH it indicates there is multiorgan failure.
3)What is the cause of death in this case?
ANS: The cause of death in this patient is might the pulmonary arrest or multiorgan failure whith uncontrolled hyperglycemia.
14) Long covid with sleep deprivation and ICU psychosis
Link to Case report log:
Questions:
1)Which subtype of ICU psychosis did the patient land into according to his symptoms?
ANS: The subtype of icu psychosis in this patient is of HYPERACTIVE
It is characterized by agitation, restlessness, emotional lability, and positive psychotic features such as hallucinations, illusions that often interfere with the delivery of care.It is not because of any primary illnes.It might be beacuase any feel of anxity and there might be cause of pharmacological and psychological casue which should be investigated.
2)What are the risk factors in the patient that has driven this case more towards ICU pyschosis?
ANS: There are more chances for a Covid patient to be landing into ICU psychosis if patient has any history of being 1) cardiovascular diseases 2) hypertension and 3) cerebrovascular diseases.
Since this patient is a known case of htn since 2 years and had a cerebrovascular episode 2 years back , the might be the cause of factor which drive the patient into ICU psychosis.
3)The patient is sleep deprived during his hospital stay..Which do u think might be the most propable condition?
A) Sleep deprivation causing ICU pyschosis
B) ICU psychosis causing sleep deprivation
ANS: The most probable condition in this case might be SLEEP DEPRIVATION CAUSING ICU PSYCHOSIS
The anxiety or any pharmacological intervention or any care delivary system might caused sleep disturbance and thus lead to icu pyschosis:
Environmental contributors include patient care, noise, light, and medications.
Patient factors, including illness severity, SOB can also play important roles
4) What are the drivers toward current persistent hypoxia and long covid in this patient?
ANS: The pneumonia that COVID-19 causes tends to take hold in both lungs. Air sacs in the lungs fill with fluid, limiting their ability to take in oxygen and causing shortness of breath, cough and other symptoms.
While most people recover from pneumonia without any lasting lung damage, the pneumonia associated with COVID-19 can be severe. Even after the disease has passed, lung injury may result in breathing difficulties that might take months to improve.
This might be the cause for persistent hypoxia in this patient
15) Moderate Covid with comorbidity (Trunkal obesity and recent hyperglycemia)
Link to Case report Log:
QUESTIONS:
1. As the patient is a non- diabetic, can the use of steroids cause transient rise in blood glucose?
2. If yes, can this transient rise lead to long term complication of New-onset diabetes mellitus?
3. How can this adversely affect the prognosis of the patient?
4. How can this transient hyperglycemia be treated to avoid complications and bad prognosis?
5. What is thrombophlebitis fever?
6. Should the infusion be stopped inorder to control the infusion thrombophlebitis? What are the alternatives?
16) Mild to moderate covid with hyperglycemia
QUESTIONS:
1. What could be the possible factors implicated in elevated glycated HB ( HBA1c ) levels in a previously Non-Diabetic covid patient?
2. What is the frequency of this phenomenon of New Onset Diabetes in Covid Patients and is it classical type 1 or type 2 or a new type?
3. How is the prognosis in such patients?
4. Do the alterations in glucose metabolism that occur with a sudden onset in severe Covid-19 persist or remit when the infection resolves?
5) Why didn't we start him on Oral hypoglycemic agents earlier?
17) Covid 19 with hypertension comorbidity
1)Does hypertension have any effect to do with the severity of the covid infection.If it is, Then how?
ANS: Yes, but not on a big scale, as there is damage to the endothelium and there is activation of clotting factors due to htn there is myight be the chance of formation of thrombus and lodge in any arterey casuing damage to particular organ.
2)what is the cause for pleural effusion to occur??
18) Covid 19 with mild hypoalbuminemia
QUESTIONS:
1. What is the reason for hypoalbuminemia in the patient?
ANS: In some patients, Inflammatory states invariably induce hypoalbuminemia as a consequence of increased capillary escape of serum albumin and other plasma solutes into the interstitium and into cells.As, there is constant inflammation in the patient that might be the cause of hypoalbuminemia.
It is also a marker for cardiological diseases, in X-Ray given there is cardiomegaly , hypoalbuminemia might be the marker for the cause of cardiomegaly.
2. What could be the reason for exanthem on arms? Could it be due to covid-19 infection ?
3. What is the reason for Cardiomegaly?
4. What other differential diagnoses could be drawn if the patient tested negative for covid infection?
5. Why is there elevated D-Dimer in covid infection? What other conditions show D-dimer elevation?
19) Covid 19 with first time diabetes
Questions:
1)Can usage of steroids in diabetic Covid patients increases death rate because of the adverse effects of steroids???
ANS: long term usage of steroids in the covid patients with diabetes causes harmfull effects which decrease the immune system and there is chance of attack of other fungal infections like black fungus(MUCORMYCOSIS). Which deprive the condition of the patient. The protocol is usage of short term usage of steriods, but studies show no improvement in short term usage of steriods in any patient.So, there must be careful observation of patients of diabetes and taking the treatment of steroids.
2)Why many COVID patients are dying because of stroke though blood thinners are given prophylactically???
ANS: The exact cause of the increase in clotting markers is uncertain, but it could be due to one (or a combination) of the mechanisms below:
- Endothelial cells express ACE2 protein, which the new coronavirus uses to enter cells. Because of this, the virus could directly invade and damage endothelial cells, triggering your body’s clotting mechanism.
- If endothelial cells aren’t being directly infected, damage to the tissues around them due to viral infection or your immune response could cause increased clotting.
- An increase in inflammatory molecules that your immune system produces in response to viral infection could activate clotting.
3)Does chronic alcoholism have effect on the out come of Covid infection????
If yes,how??
ANS: Yes, Drinking too much can lead to dehydration. COVID-19 infection can be associated with
vomiting and diarrhea, both conditions that can lead to dehydration, causing additional health
risks. Alcohol suppresses the release of antidiuretic hormones. Suppression of antidiuretic
hormones can result in diuresis, which is increased urination and can cause dehydration.
Drinking too much leads to impaired judgement and engagement in risky behaviors.
Specifically, it may interfere in efforts to practice social distancing and handwashing.
20) Severe Covid with Diabetes
Questions-
1. What can be the causes of early progression and aggressive disease(Covid) among diabetics when compared to non diabetics?
ANS: 👉COVID-19 is usually associated with poor glycemic control and a higher risk of ketoacidosis in diabetic patients.
👉Diabetic patients (especially those without comorbidity) had more pronounced biological abnormalities, including elevated inflammatory biomarkers [eg. C-reactive protein (CRP) and interleukin 6 (IL6)], elevated tissue enzymes [eg. lactate dehydrogenase (LDH)], and clotting abnormalities (eg. elevated D-dimer).
👉These abnormalities are related to severe multi-organ damage and to a propensity to thromboembolic events, as well as to the “cytokine storm” described as an aggravating factor of COVID-19
👉Metformin and SGLT2 inhibitors should be discontinued in patients with severe forms of COVID-19 owing to the risks of lactic acidosis and ketoacidosis
2. In a patient with diabetes and steroid use what treatment regimen would improve the chances of recovery?
ANS: GLIMIPERIDE which controls diabetes, controlling the diabetes in the normal level and in this patient there is also history of hypertension, so ANTI HYPERTENSIVES which regulates the level of blood pressure also lays an important role in improvement of patient.
Anyway the steriods and budecort combination will improve the situation of covid in the patient.
3. What effect does a history of CVA have on COVID prognosis?
ANS: As the COVID induces clots in some patients, the history of CVA has a bad prognosis in the case of covid as the clots may also cause the ischemic damage to brain which worsend the condition of a patient.
21) Covid 19 with multiple comorbidities:
1) What do you think are the factors in this patient that are contributing to his increased severity of symptoms and infection?
ANS: The co morbiditites like asthma, diabetes, and chronic kiney disease which act as a chealting agents in the mechanism of covid and increase in severity of infection and symptoms.
2) Can you explain why the D dimer levels are increasing in this patient?
ANS: Hypothesis is that probable mechanisms for the increased D-dimer in COVID-19 may be related to virus life cycle. The apoptotic processes target the endothelial cells of the vascular structure resulting in triggered coagulopathy and the ultimate result of increased D-dimer.
3) What were the treatment options taken up with falling oxygen saturation?
ANS: 1. Head elevation
2.O2 supplementation with 15 L/min
3.Neb with DUOLIN+BUDDCORT 6th hourly inj. This helps in decrease of inflammation happening in lung and to improve breathing which improves oxygen saturation
4) Can you think of an appropriate explanation as to why the patient has developed CKD, 2 years ago? (Note: Despite being on anti diabetic medication, there was no regular monitoring of blood sugar levels and hence no way to know for sure if it was being controlled or not)
ANS: The CKD is may be due to unctrollerd or unmonitoriesed diabetes or it also may be due to chronic use of NSAIDS
MECHANISM OF CKD IN NSAIDS USE:
mechanism of acute kidney injury (AKI) from NSAIDs is due to reduced renal plasma flow caused by a decrease in prostaglandins, which regulate vasodilation at the glomerular level. NSAIDs disrupt the compensatory vasodilation response of renal prostaglandins to vasoconstrictor hormones released by the body. Inhibition of renal prostaglandins results in acute deterioration of renal function after ingestion of NSAIDs.
10) Medical Education: (10 marks)
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research. A sample answer to this last assignment around sharing your experience log of the month can be seen in the link below but while this is by a student onsite in hospital and not locked down at home we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home:
MY LOG MAKING EXPERIENCE VIA TELEMEDIA
It is a case of 55yr old patient with seizure which is alloted on may 12 by DR.Vinay sir.
MAY 12: The case was discusseed by the sir, and contacted patient and taken a detailed history of patient.
MAY13 : All the investigations and examinations reports and interpretations are taken from the sir.
MAY 14 : Detailed study regarding the seizures and in around the casse are discussed.
This gives a alternative way in this pandemic situatioon but it is slightly unsatisfactory while coming to the patients perception. And we also tried to collect as much as possible, but it depends on the interest of the patient in tellimg the history to us.It is slightly difficult when compared to live history taking. while coming to investingations and examinations ,it is well guided by our proffessors and PGs. But we cannot perform any test or any examination. so that might be backing for us.
Thanks for all the staff who have supported me and guided us through all the ways in making the elogs and online discussuions which helped us in gaining the knowledge.





Comments
Post a Comment