GEN MED CASE 3: 55 yrs old male patient with came with cheif complaints of abdominal pain since 5 days and chest pain since 2 days
Student- A. Rishi koundinya
Batch- 2017
This is an online e log book to discuss our patient de-identified health data shared after taking his/her/guardians signed informed consent.
Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evidence based input
This E blog also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
CHEIF COMPLAINTS:
Patient came with cheif complaints of abdominal pain since 4 days and chest pain since 2 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 1 week back and then he consumed alcohol(650ml) for 2 days continuously and he developed abdominal pain which is dragging type,non radiating.
C/o chest pain dragging type,non radiating to left arm.
C/o vomiting 3 days back .
Past history:-
There is similar episodes in the past with abdominal pain, vomiting since 2 years at the time of alcohol consumption only. And it is treated with IV fluids at local hospital.
Patient is k/c/o DM since 2 yrs and on oral hypoglycemic drugs.
Personal history:-
Diet - mixed
Appetite- normal
Sleep - adequate
Bowel and bladder movements - regular.
Alcohol consumption since 30 yrs and currently consumes 650 ml of alcohol daily.
Smoking (beedi) since 10 years 3 per day.
On examination, patient is conscious, irritable and with altered sensorium.
Vitals:-
BP- 120/70 mmHg
PR-111bPm
Spo2- 99%at RA.
GRBS- 600
.
CLINICAL PICTURES:
Systemic examination:-
CNS- patient is in altered sensorium, irritable and irrelevant talk
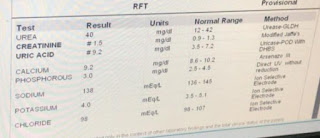
INVESTIGATIONS:-
On day 1 insulin 6 units of insulin is given.
Grbs -
5:30-600
7:30- 390
8:30-380
9:30- 383
10:30- 382
11:30- 260
12:30- 210
1:30- 220
2:30- 206
3:30- 207
4:30- 147
5:30- 77
6:30- 121
7:30- 131
Day 2
S: pt is in altered state of sensorium and irritable
Irrelevant talk
No fever spikes
O: pt is on insulin infusion @4ml/hr
Grbs:100mg/dl
Bp:120/80mmhg
PR: 94bpm
Spo2: 99%@room air
RR : 20
Grbs values:
8:30 am-100
A: DKA with k/c/o DM
P:
IVF- NS- 1L for 3hrs.
2. Inj insulin is given
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.
Treatment:-
1. IVF- NS- 1L for 3hrs.
2. Inj insulin is given.
3. GRBS monitoring hrly.
4.IVF-5% Dextrose if GRBS<250mg/dl.
5.Inj THIAMINE 100mg in 100 ml NS/IV/BD.
6.Inj OPTINEURON 1 amp in 100ml NS/IV/OD.
PROVISIONAL DIAGNOSIS:-
Diabetic ketoacidosis with known case of diabetes milletus.













Comments
Post a Comment