49 yr male with abdominal pain
This is an online E - log book to discuss our patients de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online portfolio and your valuable inputs on the comment box.
Chief complaints:
Abdominal pain since 20 days
Vomitings since 20 days
Shortness of breath since 20days
Constipation since 7days
HOPI:
Patient is apparently asymptomatic 7 years back, he complained of stomach pain since 7 days which is pricking type and radiating to back it is not associated with nausea,vomiting.
He went to the hospital and given IV fluids with analgesics and got relieved.
One month back he is complaining of abdominal pain which is pricking type and radiating and associated with decreases in appetite and vomitings(2episodes /day)Since 20 days which is non bilious and content is food particles. He went to hospital at nakerekal and underwent endoscopy.
As he is not taking any food and there is a hypoglycemia attack and dizziness is experienced by patient.and admitted to hospital.
Patient is complaining of difficulty in passing stools, he is only passing stools when he is on laxative and stools are story hard and pallets in nature , there is no complaints of farting.
PAST HISTORY:
He is known a known case of diabetes since 3 yrs and on regular medication
He is known patient of tuberculosis 10 years back and treated with medication for 9 months and relieved.
1 year ago he consulted ortho with chief complaints of left lower limb pain at knee.. there is history of fall on road while walking.
Not a k/c/o HTN, EPILEPSY OR ASTHMA
PERSONAL HISTORY:
He has mixed diet
Normal appatite
Adequate sleep
Decreased bowel movements and regular bladder .
Consuming tobacco since 10yrs
He is taking alcohol and toddy since 10yrs which is weekly twice and amount of 90ml if alcohol, 1000ml if toddy.
And he stopped taking alcohol since 1yr.
GENERAL EXAMINATION:
Pt is conscious coherent and well orientated to time place and person.
There is no pallor, icterus , clubbing, cyanosis, lymphadenopathy, edema
CVS: S1 S2 heard
R/S: BAE+
P/A:
Shape of abdomen: scaphoid with normal contour, abdomen moving with respiration, there are no scars, swellings , sinuses, no visible peristalisis and no visible pulsations, no local rose of temperature, no tenderness,no cough impulse, no organomegaley, no swellings palpable, no gaurding/ridgidity, rebound tenderness,
Diagnosis:
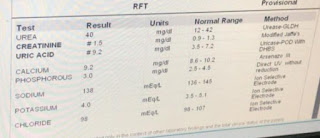
Chronic pancreatitis with type 2 diabetes mellitus since 3yrs with de-myelinating neuropathy in both lower limbs and old TB case.
Treatment:
1) IV FLUIDS NS@100ml/hr infusion
2) IV FLUIDS 0.9%NS @50ml/hr infusion
3) GRBS charting.
4) INJ. OPTINEURON 1amp in 100ml NS OD
5) INJ. PAN40mg IV/OD















Comments
Post a Comment