70 year female with sob
This is an online E - log book to discuss our patients de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patient’s clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online portfolio and your valuable inputs on the comment box.
Chief complaints:
Shortness of breath grade 4, from 10 days ,fever from 10 days,loss of appetite from 6 days ,burning micturition from 4 days,decrease urine output s from 4 days.
History of presenting illness:
Patient was apperantly asymptomatic 10 days back then she had SOB grade 4 and fever which is intermittent associated with rigors and chills and relieved on medication.
Patient was taken to hospital 8 days back and diagnosed as typhioid and was treated for the same.
Patient c/o of burning micturition and decreased urine output 4 days back
History of past illness:
K/c/o dm from 15 years (treatment with metformin 500mg)
K/c/o HTN from 10 years (treatment with telmisartan 40/12.5mg)
N/k/c/o of TB,cad, epilepsy,asthma
Daily routine:
She wakes up at 5 am
She does her breakfast at 8 to9 am.daily roti.
She does her household work .
She has lunch at 1.30 pm roti or rice .
She takes rest ,
She takes her dinner around 8 pm .
She sleeps daily at 9 pm.
Family history:
No significant family history.
Personal history:
Appetite normal.
Mixed diet.
Regular bladder and bowel movements.
No allergies .
Addictions:
Alcohol taken occasionally
Tobacco smoking daily 3 times since childhood.
General examination:
Patient is c/c/c well oriented to time and place .
BP:110/80mm hg.
PR:98bpm
RR:16cpm
No pallor/icterus /cyanosis/clubbing/lymphadenopathy/
Pedal odema present which is pitting type
Abdominal swelling also present .
Systemic examination:
Cvs:S1,s2heard.
No thrills and cardiac murmurs
Respiratory system;
Dyspnea:present
No wheezing
Position of trachea central
Breath sounds vescicular
BAE +ve
Per abdomen :
Soft ,non tender,swollen
No palpable mass
Liver and spleen not palpable.
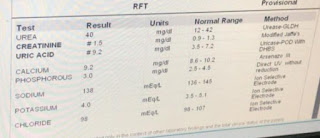
Investigations:
Provisional diagnosis:
AkI on CKD.
Treatment:
Inj .piptaz 2.25 mg iv/tid
Inj neomal 1 mg iv/sos(if temp >101°F)
Tab lasix 40 mg po/bd
Tab nodosis 500 mg po
Tab orofer -xt po/od
Tab shelcal 500 mg po /od
Tab pcm 500 mg po/sos
Capsule bio D3 po/ weekly twice







Comments
Post a Comment